New tests seek to predict liver cancer relapse and improve survival rates
Curtin University researchers will develop a suite of tissue and blood-based diagnostic tests that can predict whether liver cancer will return, giving hope to thousands of patients who currently have a less than 20 per cent chance of survival at five years.
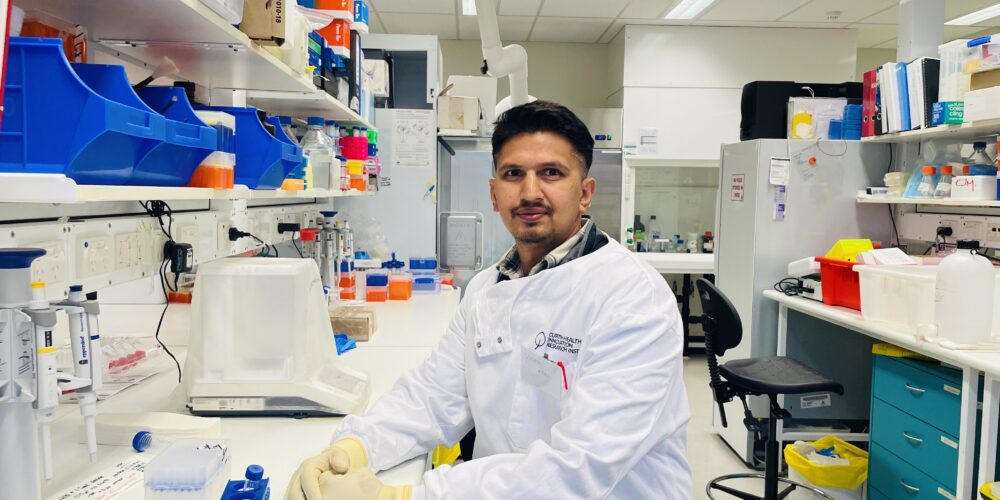
The project, led by Dr Ankur Sharma from the Curtin Medical School in partnership with leading genomics organisation BGI-Australia, was made possible by Federal Government funding of almost $1 million from the National Health and Medical Research Council’s Medical Research Future Fund Early to Mid-Career Researchers grant, announced today.
Dr Sharma said the team would develop a suite of diagnostic tests, called TRACKERx, that identify biomarkers associated with relapse in early-stage hepatocellular carcinoma (HCC) – a type of primary liver cancer.
“We will develop these TRACKERx tests by using state-of-the-art technologies to identify cells associated with the return of liver cancer, which is the fastest-growing cause of cancer-associated deaths in Australia,” Dr Sharma said.
“These tests can then be used to predict relapse and guide therapy (including immunotherapy) for HCC patients after they have undergone surgery, effectively enabling clinicians to deliver the right interventions at the right time for the right patients.
“This project builds on our team’s recent landmark findings identifying foetal-like cells in liver cancers and linking these to the cancer returning. It is the next step in translating our research into positive real-world outcomes for cancer patients.”
The Federal Government support was matched by $1.5 million from five partner organisations including Curtin University, the Liver Cancer Collaborative, BGI-International, MGI-Australia and the Harry Perkins Institute of Medical Research.
Curtin University Deputy Vice-Chancellor Research Professor Chris Moran commended the team on being awarded funding support.
“This project has the potential to save lives by reducing the high-recurrence rate for liver cancer patients after their treatment and provides the ideal pathway for this talented team of early and mid-career researchers to become future world leaders in liver cancer research,” Professor Moran said.
The project will bring together research collaborators across Australia, including from Curtin University, the Harry Perkins Institute of Medical Research, Westmead Institute for Medical Research, BGI Australia, Imperial College of London, Institute of Liver and Biliary Sciences and Sir Charles Gairdner Hospital.
The team hopes to launch the early version of the TRACKERx test in the next three to four years.
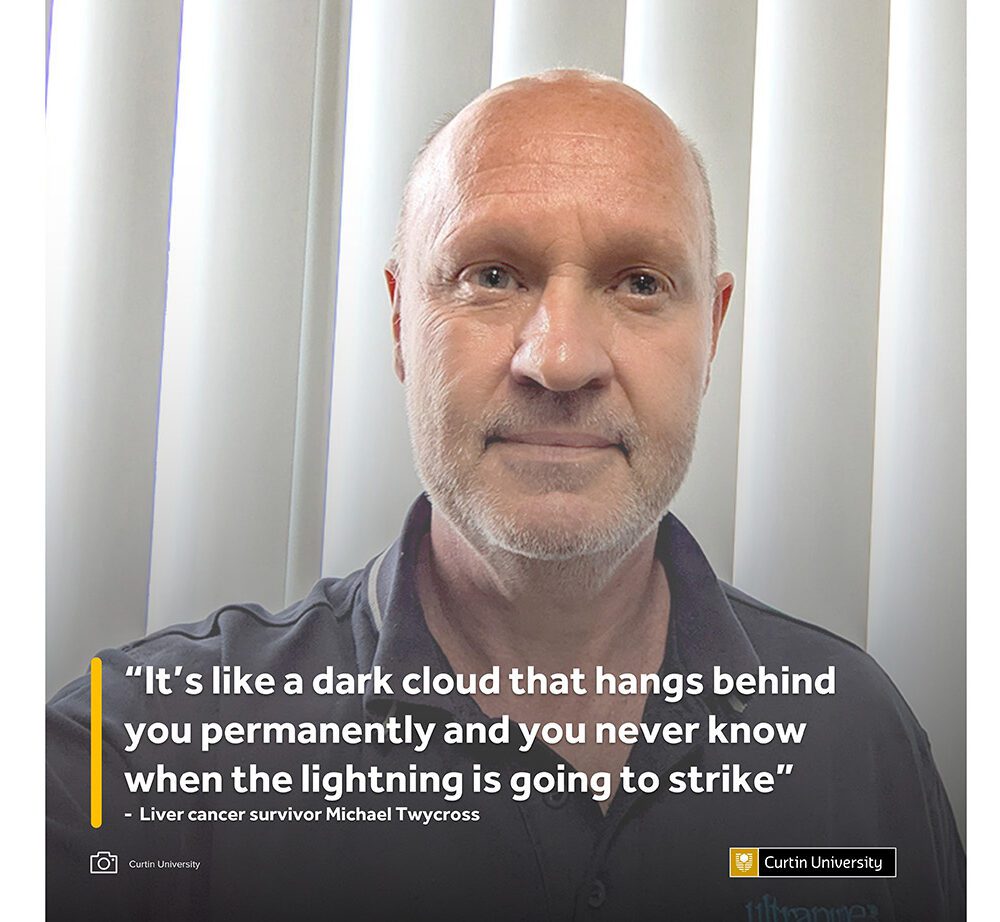
Michael Twycross, a 56-year-old small business owner from Blacktown in Sydney, was diagnosed with liver cancer in late 2021 during the COVID pandemic, following a routine blood test from his GP that saved his life.
Once he was finally referred to a specialist amid the delays caused by COVID, his tumour was removed immediately and he was advised that he was at a high risk of the cancer returning.
Since February 2022, Mr Twycross has been taking part in a trial for a new immunotherapy boosting drug that enables him to be monitored more frequently than most liver cancer survivors, but he admits the threat of the cancer returning is never far from his thoughts.
“It’s like a dark cloud that hangs behind you permanently and you never know when the lightning is going to strike,” Mr Twycross said.
“For me, any initial testing that they can do to find a recurrence early would be an absolute godsend – it would be the best thing ever. Let’s not wait until there’s a giant tumour that we have to address – let’s have a look at a couple of cells that we can hopefully step on quickly, cheaply and without too many side effects. It’s a fantastic idea. And if it is to return and they could pick it up early enough, it would be better to treat that patient while they’re still fit and healthy than wait until they are suffering the effects of cancer and then try to treat it when you’re weaker and not able to recover so well.
“Some treatments may even be taken off the table if you wait too long. It just all makes perfect sense. If you could have something to tell you as soon as possible, as soon as it could be detected, it would not only give the patient invaluable notice of what’s coming but could also give the clinicians potentially more treatment options. That, coupled with huge potential savings to the government in treating costs, turns this into a technology, where all involved could benefit greatly. In my opinion, the sooner it’s available, the better.”
For more information about the NHMRC MRFF Early to Mid-Career Researchers grants, visit here.